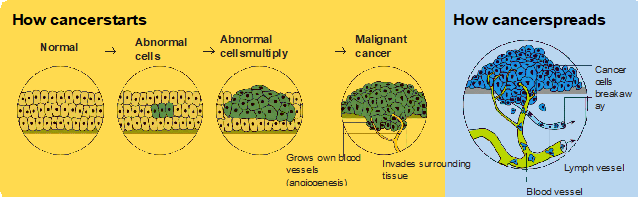
Cancer is a disease of the cells. Cell are the body’s basic building blocks - they make up tissues and organs. The body constantly makes new cells to help us grow, replace worn-out tissue and heal injuries.Normally, cells multiply and die in an orderly way, so that each new cell replaces one lost. Sometimes, however, cells become abnormal and keep growing. In solid cancers, such breast or prostate cancer, the abnormal cells form a mass or lump called a tumour. In some cancers, such as leukaemia, the abnormal cells build up in the blood.
Not all tumours are cancer. Benign tumours tend to grow slowly and usually don’t move into other parts of the body or turn into cancer. Cancerous tumours, also known as malignant tumours, have the potential to spread. They may invade nearby tissue, destroying normal cells. The cancer cells can break away and travel through the bloodstream or lymph vessels to other parts of the body.
The cancer that first develops is called the primary cancer. It is considered localised cancer if it has not spread to other parts of the body. If the primary cancer cells grow and form another tumour at a new site, it is called a secondary cancer or metastasis. A metastasis keeps the name of the original cancer. For example, pancreatic cancer that has spread to the liver is called metastatic pancreatic cancer, even though the main symptoms may be coming from the liver.
Most cancers are treated with surgery, chemotherapy and/ or radiation therapy (radiotherapy). Other drug treatments, such as hormone therapy, targeted therapy and immunotherapy, can also be used for some types of cancer. The different treatments may be used alone or in combination.
The treatments you have depend on several factors, including:
A: Chemotherapy (sometimes just called “chemo”) is the use of drugs to kill or slow the growth of cancer cells. The drugs are called cytotoxic, which means toxic to cells (cyto). Some of the drugs come from natural sources such as plants, while others are completely made in a laboratory.
A: All cells in the body grow by splitting into two cells or dividing. Chemotherapy damages cell that are dividing rapidly. Most chemotherapy drugs enter the bloodstreams and travel throughout the body to target rapidly dividing cancer cells in the organs and tissues. This is known as systemic treatment. Sometimes chemotherapy is delivered directly to the cancer. This is known as local chemotherapy.
A: You might have treatment with a single chemotherapy drug or a combination of several drugs. There are many different types of chemotherapy drugs, and each type destroys or shrinks cancer cells in a different way.
The chemotherapy drugs you have depends on the type of cancer. This is because different drugs work on different types of cancer. Sometimes chemotherapy is the only treatment needed, but you may also have surgery, radiation therapy or other drug therapies chemotherapy, and it may be given with other drug therapies.
A: Chemotherapy can be used for different reasons:
A: Chemotherapy works on cells that are dividing rapidly. Cancer cells divide rapidly, as do some healthy cells. These include cells in your blood, mouth, digestive system and hair follicles.
Side effects occur when chemotherapy damages these normal cells. Unlike cancer cells, normal cells can recover, so most side effects are temporary. The drugs used for chemotherapy are constantly being improved to give you the best possible outcomes and to reduce potential side effects.
A: Chemotherapy is most often given via a vein (intravenously). It is sometimes given in other ways, such as tablets you swallow (oral chemotherapy), as a cream, or as injections into different parts of the body. The choice depends on the type of cancer being treated and the chemotherapy drugs being used.
A: Having a needle inserted for intravenous chemotherapy may feel like having blood taken. If you have a temporary tube (cannula) in your hand or arm, only the initial injection may be uncomfortable. If you have a central venous access device, it should not be painful. Your oncologist will let you know which method is suitable.
A: Most people have chemotherapy during day visits to a hospital or treatment centre. In some cases, an overnight or extended hospital stay may be needed. People who use a portable pump or have oral chemotherapy can have their treatment at home. Sometimes a visiting nurse can give you intravenous chemotherapy in your home. Your treatment team will discuss which options are available to you.
A: How often and for how long you have chemotherapy depends on the type of cancer you have drugs that are used. You will usually have a number of treatment cycles, and these may be daily, weekly or monthly.
Often people have chemotherapy over 6-12 months, but it’s possible to have it for a shorter or longer period. Maintenance chemotherapy (to control the cancer or relieve symptoms) may last many months or years.
Sometimes it is difficult to decide on the type of treatment to have. You may feel that everything is happening too fast, or you might be anxious to get started. Check with your specialist how soon treatment should begin - often it won’t affect the success of the treatment to wait a while. Ask them to explain the options, and take as much time as you can before making a decision.
A: During chemotherapy you will be cared for by a range of health professionals who specialise in different aspects of your treatment. This is called a multidisciplinary team (MDT) and it may include some or all of the professionals listed below.
*Note that only some patients see a cancer care coordinator. It is important to maintain or develop a relationship with a general practitioner (GP). This health professional will be involved in your ongoing care, particularly once the cancer treatment finishes.
| General Practioner (GP) | Assists you with treatment decisions and works in partnership with your specialists in providing ongoing care. |
| Medical Oncologistor Haematologist: | Treats cancer with drug therapies such as chemotherapy, targeted therapy and immunotherapy (these are known a systemic treatments). |
| Radiation Oncologist | Treats cancer by prescribing and overseeing a course of radiation therapy. |
| Onco-Surgeon | Surgically removes tumours and performs some biopsies; specialist cancer surgeons are called surgical oncologists. |
| Cancer Care Coordinator | Coordinates your care, liaises with other members of the MDT, and supports you and your family throughout treatment; may also be a clinical nurse consultant (CNC) or clinical nurse specialist (CNS) |
| Nurse | Administers drug, including chemotherapy, and provides care, information and support through your treatment. |
| Palliative care specialist and nurses | Work closely with the GP and oncologist to help control symptoms and maintain quality of life. |
| Pharmacist | Dispenses medicines and gives advice about dosage and side effects. |
| Dietitian /Nutritionist | Recommends aneating plan to follow while you are in treatment and recovery. |
| Social worker | Links you to support services and helps you with emotional, practical or financial issues. |
| Occupational therapist /Physiotherapist | Assist with physical and practical problems, including restoring movement and mobility after treatment and recommending aids and equipment. |
| Psychologist / counsellor | Help you manage your emotional response to diagnosis and treatment. |